By Sonya Worthy Okolo, PT and Victoria Hudson, SPT
Dyspareunia or pain with sex is more common than you may think. In the U.S. 10-20% of women experience pain with sex and nearly 1 in 4 women experience pain with sex over their lifetime. So let’s dive into why is sex painful for you…
Everyone may experience pain in different ways. Whether it be with shallow or deep penetration, manual touch, pain with particular positions, spasms with orgasms, or throbbing and aching after sex. They are all common, but not normal to healthy sexual activity. It could be a nerve, muscle, hormone, or tissue issue. Additionally, we cannot forget the emotional factors affecting our sexual experiences. Mental health conditions, such as anxiety or depression, uncontrolled stress, and a history of sexual abuse can lead to pain with sex.
Sexual Intercourse can become painful for a number of reasons…do you know YOUR WHY?
If pain with entry:
- Lack of lubrication in the vagina from lack of foreplay, drop in estrogen after menopause/ breastfeeding, medication side effects (including birth control pills!)
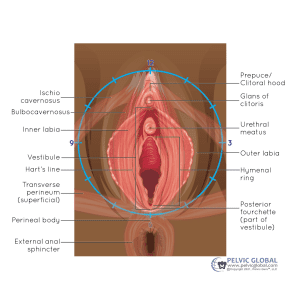
- Anatomical issues such as clitoral phimosis, imperforate hymen, or Congenital Neuroproliferative Vestibulodynia
- Irritation or injury to the vaginal tissues following trauma, surgery, or childbirth
- Skin problems, urinary tract or genital infections may cause pain and inflammation
- Fear causing Vaginismus, an involuntary spasm of muscle within vaginal wall with penetration
If deep pain with sex:
- Certain abdomino-pelvic conditions such as Endometriosis, Interstitial Cystitis, Pelvic Inflammatory Disease, Fibroids, and Irritable Bowel Syndrome
- Altered anatomy, such retroverted uterus or pelvic organ prolapse
- Post-surgical scarring from organ removal, deep incisions, or cancer treatment
How can sex be enjoyable again?
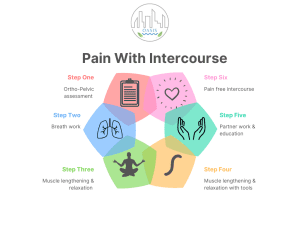
The Oasis 3R method (Restore, Retrain, Reintegrate) begins with a comprehensive evaluation to identify contributing factors to pain. This includes a review of past medical history, menses story and patterns, medications, and lifestyle screen. The physical exam will assess and identify muscle, nerve, and tissue function and irritability.
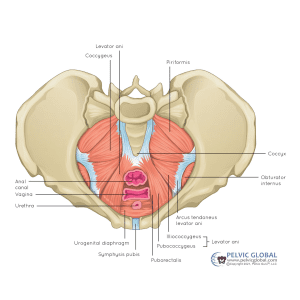
Treatment by a Pelvic Floor Therapist involves techniques and tools to address muscle dysfunction, reduce pain, retrain nervous system response, and mind-body connection to pelvis.
- Can your muscles contract and relax?
- Is there muscle coordination needed for orgasm?
- Are strategies needed for mechanics of intercourse pending issues?
Given your unique history and exam, we will develop a personalized treatment plan. This may include collaboration with other necessary health care team members. Adaptive tools may be recommended for self-directed pelvic floor muscle lengthening and relaxation. Also, education on positions, props, and/or devices may be needed.
Your emotional comfort AND physical comfort are equally important as we work towards goals. As you work with your Pelvic Floor Therapist, it is important to also understand the role of your nervous system.
Consider these resources:
“Come As You Are” by Emily Nagoski, PhD
“Reviving Your Sex Life After Childbirth: Your Guide to Pain Free & Pleasurable Sex After Baby” by Kathe Wallace, PT, BCB-PMD
“Better Sex Through Mindfulness: How Women Can Cultivate Desire” by Lori A Brotto, PhD
“Wanting Sex Again: How to Rediscover Your Desire and Heal a Sexless Marriage” by Laurie J Watson, LMFT, LPC, Certified Sex Therapist
Ready to put an end to painful sex? Help is available for your most intimate concerns!
Call 301-381-4551 to schedule a comprehensive Pelvic Floor Evaluation.

